| |
| Med Sci (Paris). 34: 39–42. doi: 10.1051/medsci/201834f107.Incidence and risk factors of the temporomandibular joint disorders in the patients without condylar fractures Yan Junjie,1 Liu Weidong,1 Lin Ren,1 and Ye Min1* 1Department of stomatology, Lishui people’s hospital (6th affiliated hospital of Wenzhou medical university) Zhejian Lishui, No.15 Dazhong Road, Liandu District, Lishui City, Zhejiang Province323000PR China. |
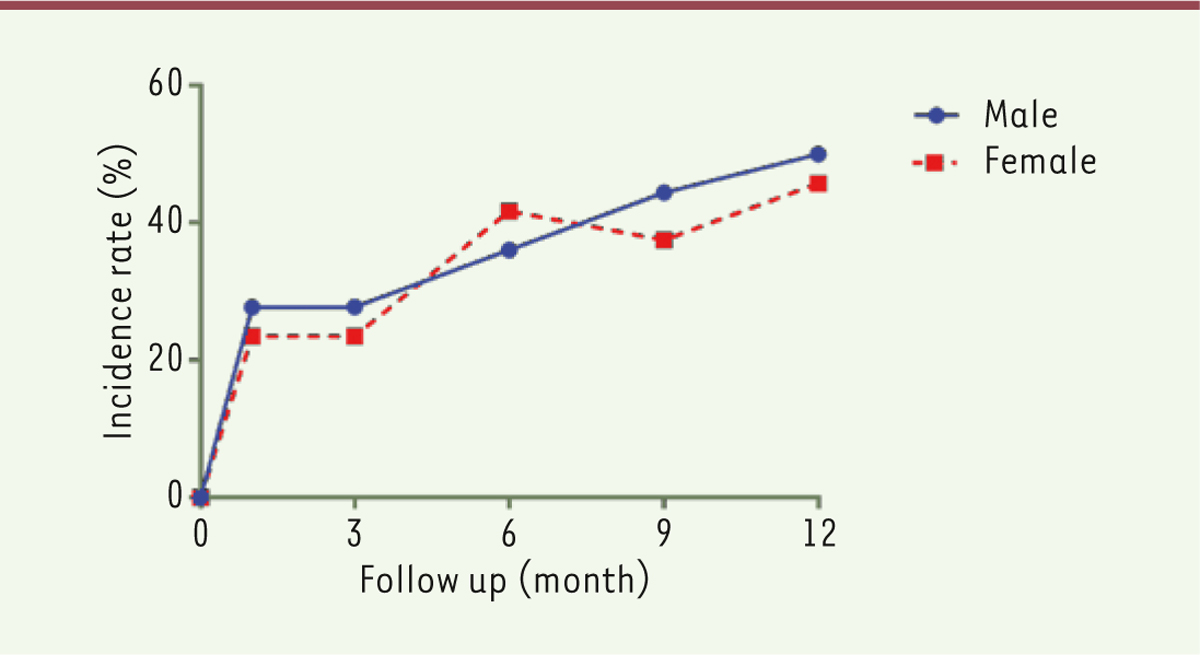
Objective: To evaluate the incidence and risk factors of the temporomandibular joint disorders (TMD) in the patients suffering from maxillo-facial injury without condylar fractures. Methods: sixty patients without condylar fractures were recruited from Feb 2014 to Nov 2015 in the department of stomatology, Lishui people’s hospital. The incidence of TMD was recorded at 1, 3, 6, 9 and 12 months after injury through MRI examination. The risk factors for TMD were evaluated by logistic regression analysis. Results: the TMD incidence rates were 25.0%, 30.0%, 35.0%, 41.7% and 48.3% at 1, 3, 6, 9 and 12 months after injury with no statistical difference between male and female (P>0.05). Logistic regression indicated that disorder of occlusal relationship (OR=1.84,95%CI:1.36-2.78) and hemi-mastication (OR=1.56, 95% CI:1.23- 2.24) were independent risk factors for the development of TMD. Conclusion: there was a high incidence of temporomandibular joint disorders in the patients suffering from maxillo-facial injury without condylar fractures. The disorder of occlusal relationship and hemi-mastication were independent risk factors for the development of post-injury TMD. Keywords: incidence, logistic regression, risk factors, temporomandibular joint disorders, trauma |
Maxillofacial region suffers from injury particularly in patients with knocked jawbone. In the absence of condylar fractures, the injury of the temporomandibular joint is easily overlooked. Without timely and effective treatment, patients often suffer from temporomandibular joint disorders (TMDs), such as joint ringing, mouth opening difficulty, and ankylosis over time, which severely affect their quality of life [1-3]. TMD is an umbrella term covering pain and dysfunction of the muscles of mastication (the muscles that move the jaw) and the temporomandibular joints (the joints which connect the mandible to the skull). The most important feature is pain, followed by restricted mandibular movement. At present, scholars in China have rarely evaluated TMD and studied its epidemiological data in patients without traumatic condylar fractures caused by accidents [4]. In the present work, we conducted an observation study of patients suffering from maxillofacial injuries treated in our hospital over the recent 2 years. Through CT and MRI examinations of the temporomandibular joint, we evaluated the incidence and relevant risk factors in patients with TMD but without traumatic condylar fractures. The purpose of this study was to provide some information for investigating the progression, evolution, prevention, diagnosis, and treatment of TMD. |
Patients From February 2014 to November 2015, the Stomatology Department of Lishui People’s Hospital received 60 patients with maxillofacial trauma but without condylar fractures. Patients who satisfied the following criteria were included: age of 18 years or older; presence of evident maxillofacial trauma; lack of condyle fracture, as determined through CT or MRI examination; and signature of informed consent for voluntary joining of the clinical study. The exclusion criteria are as follows: age less than 18 years; unobvious trauma; presence of condyle fracture and oral and maxillofacial deformity.
Table 1
| Factors |
Variable |
Assignment |
| TMD |
Y |
Negative, Y=0; Positive, Y=1 |
|
| Age |
X1 |
≤40 year, X1=0; 40 year, X1=1 |
|
| Gender |
X2 |
Male, X2=0; Female, X2=1 |
|
| Disorder of occlusal relationship |
X3 |
Negative, X3=0; Positive, X3=1 |
|
| Open mouth habit |
X4 |
Negative, X4=0; Positive, X4=1 |
|
| Hemi-mastication |
X5 |
Negative, X5=0; Positive, X5=1 |
|
| bruxism |
X6 |
Negative, X6=0; Positive, X6=1 |
|
| Mental factors |
X7 |
Negative, X7=0; Positive, X7=1 |
|
| History of orthodontic |
X8 |
Negative, X8=0; Positive, X8=1 |
The value of independent variables and dependent variables in the Logistic regression equation.
|
Data Collection Data were collected through consultation, clinical examinations (evaluation of soreness or soreness of joints, joint snapping, and jaw dyskinesia), and physical examinations (assessment of joint acoustics, dyscinesia, pain, joint, and muscles). Clinical examinations included evaluation of mandibular edge movement (maximal opening, maximal forward extension, and maximal lateral movement); joint dysfunction; pain in jaw movement; pain in masticatory muscles (chewing muscle palpation involves deep and shallow chewing muscles, medial pterygoid muscles, lateral pterygoid muscles, anterior, middle and posterior temporalis); and joint pain (joint palpation involves extra-joint and posterior joint). Follow-up Post-traumatic patients were followed-up through telephone appointment and MRI and clinical examinations in January, March, June, September, and December. After the appointment, TMJ Helkimo index evaluation and MRI examination were conducted to determine whether or not patients suffer from TMD. Diagnostic criteria The diagnostic criteria for TMD include the Helkimo index [ 5, 6] , the anamnestic dysfunction index (Ai) for MRI imaging of temporomandibular joint, and the clinical dysfunction index (Di) [ 7, 8]. Statistical analysis Data were analyzed using the SPSS17.0 statistical software. Measurement data were expressed with  and the comparison between groups was made based on the t-test of the sample mean. The enumeration data were expressed with a relative number, and the comparison between groups was made based on the χ 2 test. The parameters with significant difference analyzed by t-test or χ 2 test were further included in the logistic regression equation to screen the independent factors relevant to risk factor for TMD. P value <0.05 was considered as statistical significant. |
Incidence of TMD. Sixty patients were followed-up for 1 year after injury. The incidence rates of TMD at 1, 3, 6, 9 and 12 months were 25.0%, 30.0%, 35.0%, 41.7% and 48.3%, respectively. No significant difference in the incidence was found between male and female patients (P < 0.05, Figure 1).
 | Figure 1. Incidence of TMD during 12 months post-injury. |
Relevant factor for temporomandibular joint disorders Single factor chi-square analysis showed that open mouth habit (P<0.05), hemi- mastication (P<0.05) and bruxism (P<0.05), (Table 2) were correlated with the development of TMD.
Table 2
| Factors |
TMD(n=29) |
Non-TMD(n=31) |
P |
| Gender |
|
|
>0.05 |
|
| Male |
17 |
19 |
|
|
| Female |
12 |
12 |
|
|
| Age (year) |
42.3±11.2 |
44.1±12.6 |
>0.05 |
|
| ≤40 |
12 |
13 |
|
|
| >40 |
17 |
18 |
|
|
| Disorder of occlusal relationship |
|
|
<0.05 |
|
| Positive |
6 |
0 |
|
|
| Negative |
23 |
31 |
|
|
| Open mouth habit |
|
|
<0.05 |
|
| Positive |
9 |
1 |
|
|
| Negative |
20 |
30 |
|
|
| Hemi-mastication |
|
|
<0.05 |
|
| Positive |
12 |
3 |
|
|
| Negative |
17 |
28 |
|
|
| Bruxism |
|
|
<0.05 |
|
| Positive |
7 |
1 |
|
|
| Negative |
22 |
30 |
|
|
| Mental factors |
|
|
>0.05 |
|
| Positive |
4 |
0 |
|
|
| Negative |
25 |
31 |
|
|
| History of orthodontic |
|
|
>0.05 |
|
| Positive |
3 |
1 |
|
|
| Negative |
26 |
30 |
|
Potential risk factors for temporomandibular joint disorders after oral and maxillofacial trauma.
|
Independent risk factors for TMD Logistic regression test showed that occlusion disorder (OR=1.84, 95%CI: 1.36-2.78) and hemi-mastication (OR=1.56, 95%CI:1.23-2.24) are independent risk factors for the development of TMD |
TMD frequently occurs in oral and maxillofacial regions and has an incidence rate of about 25% in general population [3]. TMD is often associated with occlusion disorders, headache, neck pain, hearing loss, or even facial deformities, which severely affect the quality of life of patients[1, 9]. An epidemiology study reported that the incidence rate of TMD in the Chinese population is 21.2%-40% [10], which is close to the worldwide incidence rate. The pathogenesis of TMD includes autoimmunity, trauma, infection, developmental disorder, and tumor. Among patients with injured mandibular jaws, 1/3 of them suffer from delayed temporomandibular joint disorders [11]. Factors, such as occlusal relation and airway abnormalities, play a critical role in the pathogenesis of TMD [12, 13]. Traumas associated with the temporomandibular joint area are not usually characterized by condylar fractures but include injury of ligaments, articular cartilage, articular discs and associated bones, and masticatory muscles. They may lead to changes in the biochemical environment of the joint and to the occurrence of oxidative stress and free radicals; as a result, a series of aseptic inflammation occurs, thereby changing the original normal structure of the joint and causing functional changes [14]. Animal model experiments have shown that traumatic TMD is mainly characterized by pathological changes, such as osteoarthritis, followed by local micro-fractures and bone dysplasia [4]. As a scientific, effective, and noninvasive examination method, MRI is widely used in preoperative diagnosis and postoperative evaluation of TMD. Compared with CT, MRI can more clearly shows the shape and location of ligaments, cartilages, and discs in the temporomandibular joint area. MRI contrast of bilateral TMJ area can reveal subtle changes in the anatomical structures within this area after trauma. Considering these advantages of MRI, we applied it for routine examination of TMJ area to obtain imaging and determine the progression of TMD. After searching the databases, we did not find any study reporting the incidence and risk factors of TMD without condylar fractures. In the present work, we have studied the incidence and risk factors of TMD without condylar fractures and we report herein epidemiological data and related independent risk factors of TMD for the first time in China. The incidence of TMD without condylar fractures after trauma is high, and the incidence rate gradually increases with increasing follow-up time. However, no significant difference was found between male and female patients. Moreover, the incidence of TMD was high in traumatic patients who suffered from bite disorders and unilateral mastication. Hence, traumas, occlusal disorders, and unilateral mastication are independent risk factors for TMD. Patients with these characteristics should promptly remove their poor health habits to reduce the risk of TMD. Medical workers should also focus on post-traumatic patients without condyle fractures to effectively reduce the incidence of TMD. |
This work was supported by Talent lift project of Lishui People’s Hospital (2017CTB015). |
The authors declare that they have no competing interests. |
1. Badel T, C´ imic´ S, Munitic´ M, Zadravec D, Kes VB, Šimunkovic´ SK. Clinical view of the temporomandibular joint disorder . Acta Clin Croat. 2014;;53::462.–70. 2. Dugashvili G, Menabde G, Janelidze M, Chichua Z, Amiranashvili I. Temporomandibular joint disorder (review) . Georgian Med News. 2013: :17.–21. 3. Stack BC, Stack BC. Temporomandibular joint disorder . Am Fam Physician. 1992; ; 46 : :143.–150. 4. Daoying A.. Mangement of temporomandibular joint disorders . Modern Journal of Integrated Traditional Chinese and Western Medicine. 2014: :3757.–3759. 5. Suhas S, Ramdas S, Lingam PP, Naveen KHR, Sasidharan A, Aadithya R. Assessment of temporomandibular joint dysfunction in condylar fracture of the mandible using the Helkimo index . Indian J Plast Surg. 2017; ; 50 : :207.–212. 6. Rani S, Pawah S, Gola S, Bakshi M. Analysis of Helkimo index for temporomandibular disorder diagnosis in the dental students of Faridabad city: A cross-sectional study . J Indian Prosthodont Soc. 2017; ; 17 : :48.–52. 7. Pekkarinen V, Yli-Urpo A. Dysfunction of the masticatory system and the mutilated dental arch: anamnestic index, dysfunction index and occlusal index before restorative and prosthetic treatment . Proc Finn Dent Soc. 1984; ; 80 : :73.–79. 8. Helkimo M. Studies on function and dysfunction of the masticatory system. II. Index for anamnestic and clinical dysfunction and occlusal state . Sven Tandlak Tidskr. 1974;;67::101.–21. 9. Mottaghi A, Zamani E. Temporomandibular joint health status in war veterans with post-traumatic stress disorder . J Educ Health Promot. 2014; ; 3 : :60.. 10. Ningshan G, Meiqing W, Xiangquan H, Yi Z. Investigation of temporal mandibular joint disorder and tooth loss - Epidemiology . Journal of Practical Stomatology. 2000; ; 16 : :322.–324. 11. Salé H, Isberg A. Delayed temporomandibular joint pain and dysfunction induced by whiplash trauma: a controlled prospective study . J Am Dent Assoc. 2007; ; 138 : :1084.–1091. 12. Arsenina OI, Popova AV, Gus LA. The role of occlusal disorders in development of temporomandibular joint dysfunction . Stomatologiia (Mosk). 2014; ; 93 : :64.–67. 13. Ohnishi M.. Pathology and treatment of temporomandibular joint disorders: intra-articular injection therapy and arthroscopic surgery . Nihon Seikeigeka Gakkai Zasshi. 1995; ; 69 : :358.–374. 14. Yun PY, Kim YK. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder . J Oral Maxillofac Surg. 2005; ; 63 : :1576.–1583. |


 and the comparison between groups was made based on the t-test of the sample mean. The enumeration data were expressed with a relative number, and the comparison between groups was made based on the χ2 test. The parameters with significant difference analyzed by t-test or χ2 test were further included in the logistic regression equation to screen the independent factors relevant to risk factor for TMD. P value <0.05 was considered as statistical significant.
and the comparison between groups was made based on the t-test of the sample mean. The enumeration data were expressed with a relative number, and the comparison between groups was made based on the χ2 test. The parameters with significant difference analyzed by t-test or χ2 test were further included in the logistic regression equation to screen the independent factors relevant to risk factor for TMD. P value <0.05 was considered as statistical significant.